prostatitisis an inflammatory disease of the prostate gland. It manifests itself with frequent urination, pain in the penis, scrotum, rectum, sexual disorders (erection, early ejaculation, etc. ), sometimes retention of urine, blood in the urine. The diagnosis of prostatitis is established by a urologist or andrologist based on the typical clinical picture, the results of the rectal examination. In addition, an ultrasound of the prostate, back culture of prostate secretion and urine is performed. The treatment is conservative - antibiotic therapy, immunotherapy, prostate massage, lifestyle correction.
Main information
Prostatitis is an inflammation of the seminal (prostate) gland - the prostate. It is the most common disease of the genitourinary system in men. It most often affects patients aged 25-50 years. According to various data, 30-85% of men over the age of 30 suffer from prostatitis. Possible formation of an abscess of the prostate gland, inflammation of the testicles and appendages, which threatens infertility. The rise of the infection leads to inflammation of the upper genitourinary system (cystitis, pyelonephritis).
The pathology develops with the penetration of an infectious agent that enters the prostate tissue from the organs of the genitourinary system (urethra, bladder) or from a distant inflammatory focus (with pneumonia, influenza, tonsillitis, furunculosis).
Prostate adenoma is a benign neoplasm of the paraurethral glands located around the urethra in its prostatic part. The main symptom of prostate adenoma is a violation of urination due to the gradual compression of the urethra by one or more growing nodes. The pathology is characterized by a benign course.
Only a small proportion of patients seek medical help, but upon detailed examination, the symptoms of the disease are found in every fourth man aged 40-50 years and in half of men aged 50-60 years. The disease is found in 65% of men aged 60-70 years, 80% of men aged 70-80 years and more than 90% of men aged over 80 years. The severity of symptoms can vary greatly. Studies in the field of clinical andrology show that urination problems occur in about 40% of men with BPH, but only one in five patients in this group seek medical help.
Causes of prostatitis
Staphylococcus aureus (Staphylococcus aureus), Enterococcus (Enterococcus), Enterobacter (Enterobacter), Pseudomonas (Pseudomonas), Proteus (Proteus), Klebsiella (Klebsiella) and Escherichia coli (E. Coli) can act as an infectious agent in an acute process. . Most microorganisms belong to the conditionally pathogenic flora and cause prostatitis only in the presence of other predisposing factors. Chronic inflammation is usually due to polymicrobial associations.
The risk of developing the disease increases with hypothermia, a history of specific infections and conditions accompanied by congestion in the tissues of the prostate. There are the following predisposing factors:
- General hypothermia (single or permanent, related to working conditions).
- Sedentary lifestyle, profession that forces a person to be in a sitting position for a long time (computer operator, driver, etc. ).
- Constant constipation.
- Violations of the normal rhythm of sexual activity (excessive sexual activity, prolonged abstinence, incomplete ejaculation during "usual" intercourse, devoid of emotional coloring).
- The presence of chronic diseases (cholecystitis, bronchitis) or chronic infectious foci in the body (chronic osteomyelitis, untreated caries, tonsillitis, etc. ).
- Past urological diseases (urethritis, cystitis, etc. ) and sexually transmitted diseases (chlamydia, trichomoniasis, gonorrhea).
- Conditions that cause suppression of the immune system (chronic stress, irregular and malnutrition, regular lack of sleep, overtraining in athletes).
It is assumed that the risk of developing pathology increases with chronic intoxication (alcohol, nicotine, morphine). Some studies in the field of modern andrology prove that chronic perineal trauma (vibration, shock) in motorists, motorcyclists and cyclists is a provoking factor. However, the majority of experts believe that all these circumstances are not the real causes of the disease, but only contribute to the exacerbation of the latent inflammatory process in the tissues of the prostate.
Congestion in the tissues of the prostate plays a decisive role in the occurrence of prostatitis. Violation of capillary blood flow causes an increase in lipid peroxidation, edema, exudation of prostate tissues and creates conditions for the development of an infectious process.
The mechanism of prostate adenoma development is still not fully understood. Despite the widespread opinion associating the pathology with chronic prostatitis, there is no data to confirm the relationship between these two diseases. The researchers did not find a relationship between the development of prostate adenoma and the use of alcohol and tobacco, sexual orientation, sexual activity, sexually transmitted and inflammatory diseases.
There is a pronounced dependence of the frequency of prostate adenoma on the age of the patient. Scientists believe that the adenoma develops as a result of a hormonal imbalance in men during andropause (male menopause). This theory is supported by the fact that men who are castrated before puberty never suffer from pathology, and extremely rarely - men who are castrated after it.
Symptoms of prostatitis
Acute prostatitis
There are three stages of acute prostatitis, which are characterized by the presence of a certain clinical picture and morphological changes:
- Acute catarrhal. Patients complain of frequent, often painful urination, pain in the sacrum and perineum.
- Acute follicular. The pain becomes more intense, sometimes radiates to the anus, intensifies during defecation. Urination is difficult, urine comes out in a thin stream. In some cases, there is retention of urine. A subfebrile state or moderate hyperthermia is characteristic.
- Acute parenchymal. Severe general intoxication, hyperthermia up to 38-40 ° C, chills. Dysuric disorders, often - acute retention of urine. Sharp, throbbing pain in perineum. Difficulty defecating.
Chronic prostatitis
In rare cases, chronic prostatitis becomes the result of an acute process, but as a rule, a primary chronic course is observed. Sometimes the temperature rises to subfebrile values. The patient notes slight pain in the perineum, discomfort during the act of urination and defecation. The most characteristic symptom is scanty discharge from the urethra during defecation. The primary chronic form of the disease develops over a considerable period of time. It is preceded by prostatosis (blood stagnation in the capillaries), gradually turning into abacterial prostatitis.
Chronic prostatitis is often a complication of the inflammatory process caused by the causative agent of a specific infection (chlamydia, trichomonas, ureaplasma, gonococcus). Symptoms of a specific inflammatory process in many cases mask the manifestations of prostate damage. Perhaps a slight increase in pain during urination, slight pain in the perineum, scanty discharge from the urethra during defecation. A slight change in the clinical picture often goes unnoticed by the patient.
Chronic inflammation of the prostate gland can manifest itself with a burning sensation in the urethra and perineum, dysuria, sexual disorders, increased general fatigue. The consequence of potency disorders (or fear of these disorders) often becomes mental depression, anxiety and irritability. The clinical picture does not always include all the listed groups of symptoms, it is different for different patients and changes over time. There are three main syndromes characteristic of chronic prostatitis: pain, dysuric, sexual disorders.
There are no pain receptors in prostate tissue. The cause of pain in chronic prostatitis becomes almost inevitable due to the abundant innervation of the pelvic organs, the involvement of the nerve pathways in the inflammatory process. Patients complain of pain of varying intensity - from weak, aching to intense, disrupting sleep. There is a change in the nature of the pain (intensification or weakening) with ejaculation, excessive sexual activity or sexual abstinence. The pain spreads to the scrotum, sacrum, perineum, sometimes in the lumbar region.
As a result of inflammation in chronic prostatitis, the volume of the prostate increases, pressing the urethra. The lumen of the ureter is reduced. The patient has a frequent urge to urinate, a feeling of incomplete emptying of the bladder. As a rule, dysuric phenomena are manifested in the early stages. Compensatory hypertrophy of the muscle layer of the bladder and ureters then develops. Symptoms of dysuria during this period weaken and then increase again with decompensation of adaptive mechanisms.
In the initial stages, dyspotency may develop, which manifests itself differently in different patients. Patients may complain of frequent nocturnal erections, blurred orgasm or worsening erection. Accelerated ejaculation is associated with a decrease in the threshold level of arousal of the orgasmic center. Painful sensations during ejaculation can cause refusal of sexual activity. In the future, sexual dysfunctions become more pronounced. In an advanced stage, impotence develops.
The degree of sexual disorder is determined by many factors, including the sexual constitution and psychological mood of the patient. Violations of potency and dysuria can be due both to changes in the prostate gland and to the suggestibility of the patient, who, if he has chronic prostatitis, expects the inevitable development of sexual disorders and urination disorders. Psychogenic dyspotence and dysuria develop especially often in suggestible, anxious patients.
Impotence, and sometimes the very threat of possible sexual disorders, is difficult for patients to tolerate. Often there is a change in character, irritability, unpleasantness, excessive concern for one's own health and even "sickness care".
There are two groups of symptoms of the disease: irritative and obstructive. The first group of symptoms includes increased urination, constant (imperative) urges to urinate, nocturia, urinary incontinence. The group of obstructive symptoms includes difficulty urinating, delayed onset and prolonged time to urinate, feeling of incomplete emptying, urinating with an intermittent slow stream, urge to strain. There are three stages of prostate adenoma: compensated, subcompensated and decompensated.
Compensated stage
At the compensated stage, the dynamics of the act of urination changes. It becomes more frequent, less intense and less free. He needs to urinate 1-2 times at night. As a rule, nocturia at stage I of prostate adenoma does not cause concern in a patient who associates constant night awakenings with the development of age-related insomnia. During the day, the normal frequency of urination can be maintained, but patients with prostate adenoma in the first stage note a waiting period, especially pronounced after a night's sleep.
After that, the frequency of daily urination increases and the volume of urine excreted during urination decreases. There are imperative drives. The stream of urine, which had previously formed a parabolic curve, is ejected slowly and falls almost vertically. Bladder muscle hypertrophy develops, due to which the efficiency of its emptying is preserved. At this stage, there is little or no residual urine in the bladder (less than 50 ml). The functional state of the kidneys and upper urinary tract is preserved.
Subcompensated stage
In the II stage of prostate adenoma, the bladder increases in volume, dystrophic changes develop in its walls. The amount of residual urine is over 50 ml and continues to increase. During the act of urination, the patient is forced to intensively strain the abdominal muscles and the diaphragm, which leads to an even greater increase in intravesical pressure.
The act of urination becomes multiphasic, intermittent, wave-like. The passage of urine through the upper urinary tract is gradually disturbed. Muscular structures lose their elasticity, the urinary tract expands. Renal function is impaired. Patients worry about thirst, polyuria and other symptoms of progressive chronic renal failure. When the compensation mechanisms fail, the third stage begins.
Decompensated stage
The bladder in patients with stage III prostate adenoma is distended, full of urine, easily determined by palpation and visually. The upper edge of the bladder can reach the level of the navel and above. Emptying is impossible even with intense tension of the abdominal muscles. The urge to empty the bladder is constant. There may be severe pain in the lower abdomen. Urine is passed often, in drops or very small portions. In the future, the pain and the urge to urinate gradually weaken.
Characteristic paradoxical retention of urine or paradoxical ischuria develops (bladder is full, urine is constantly released drop by drop). The upper urinary tract is enlarged, the functions of the renal parenchyma are disturbed due to the constant obstruction of the urinary tract, which leads to an increase in the pressure in the pelvic-vein system. The clinic of chronic renal failure is growing. Without medical care, patients die from progressive CKD.
Complications
In the absence of timely treatment of acute prostatitis, there is a significant risk of developing a prostate abscess. With the formation of a purulent focus, the patient's body temperature rises to 39-40 ° C and can become hectic. Periods of heat alternate with severe chills. Sharp pains in the perineum make it difficult to urinate and make defecation impossible.
Increasing swelling of the prostate leads to acute urinary retention. Rarely, an abscess spontaneously ruptures into the urethra or rectum. When opened, purulent, cloudy urine with an unpleasant pungent odor appears in the urethra, when opened, feces contain pus and mucus in the rectum.
Chronic prostatitis is characterized by an undulating course with periods of prolonged remissions, during which the inflammation in the prostate is latent or manifests itself with extremely weak symptoms. Patients who are not worried about anything often stop the treatment and return only when complications develop.
The spread of the infection through the urinary tract causes the appearance of pyelonephritis and cystitis. The most common complication of the chronic process is inflammation of the testicles and epididymis (epdidymorchitis) and inflammation of the seminal vesicles (vesiculitis). The result of these diseases is often infertility.
Diagnosis
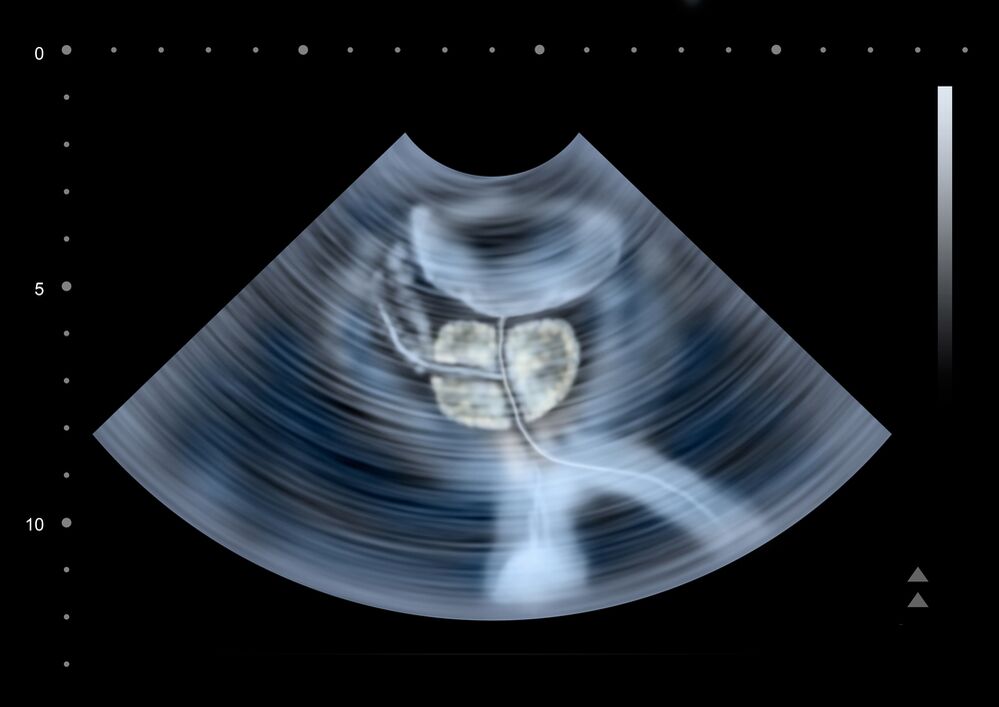
To assess the severity of prostate adenoma symptoms, the patient is asked to complete a urination diary. During the consultation, the urologist performs a digital examination of the prostate. In order to rule out infectious complications, sampling and examination of prostatic secretions and spots from the urethra is performed. Additional testing includes:
- Ultrasound.In the process of ultrasound of the prostate, the volume of the prostate gland is determined, stones and areas with congestion are detected, the amount of residual urine, the condition of the kidneys and urinary tract is assessed.
- Urodynamic study.Uroflowmetry allows you to reliably assess the degree of urine retention (the time of urination and the rate of urine outflow are determined by a special device).
- Definition of tumor markers.To exclude prostate cancer, it is necessary to evaluate the level of PSA (prostate specific antigen), the value of which should not normally exceed 4 ng / ml. In controversial cases, a biopsy of the prostate is performed.
In recent years, cystography and excretory urography in prostate adenoma are performed less frequently due to the emergence of new, less invasive and safer research methods (ultrasound). Sometimes cystoscopy is performed to exclude diseases with similar symptoms or in preparation for surgical treatment.
Treatment of prostatitis
Treatment of acute prostatitis
Patients with an uncomplicated acute process are treated by a urologist on an outpatient basis. In case of severe intoxication, suspected purulent process, hospitalization is indicated. Antibacterial therapy is administered. Preparations are selected taking into account the sensitivity of the infectious agent. Antibiotics are widely used and can penetrate the prostate tissue well.
With the development of acute retention of urine against the background of prostatitis, they resort to installing a cystostomy rather than a urethral catheter, as there is a danger of prostate abscess formation. With the development of an abscess, endoscopic transrectal or transurethral opening of the abscess is performed.
Treatment of chronic prostatitis
Treatment of chronic prostatitis should be complex, including etiotropic therapy, physiotherapy, correction of immunity:
- Antibiotic therapy. The patient is prescribed long courses of antibacterial drugs (within 4-8 weeks). The choice of the type and dosage of antibacterial drugs, as well as the determination of the duration of the course of treatment, is made individually. The drug is selected based on the sensitivity of the microflora according to the results of the culture of urine and prostate secretion.
- Prostate massage.Massage of the gland has a complex effect on the affected organ. During the massage, the inflammatory secretion accumulated in the prostate gland is squeezed into the channels, then enters the urethra and is removed from the body. The procedure improves blood circulation in the prostate, which minimizes congestion and ensures better penetration of antibacterial drugs into the tissue of the affected organ.
- Physiotherapy.Laser exposure, ultrasound waves and electromagnetic vibrations are used to improve blood circulation. If it is impossible to carry out physiotherapy procedures, the patient is prescribed warm medicinal microclysters.
In case of chronic, prolonged inflammation, a consultation with an immunologist is indicated for choosing the tactics of immunocorrective therapy. The patient is given advice on lifestyle changes. Changing the lifestyle of a patient with chronic prostatitis is both a curative and preventive measure. The patient is recommended to normalize sleep and wakefulness, establish a diet, conduct moderate physical activity.
Conservative therapy
Conservative therapy is carried out in the early stages and in the presence of absolute contraindications for surgery. To reduce the severity of the symptoms of the disease, alpha-blockers, 5-alpha reductase inhibitors, herbal preparations (extract from African plum bark or sabal fruit) are used.
Antibiotics are prescribed to fight the infection that often accompanies prostate adenoma. At the end of the course of antibiotic therapy, probiotics are used to restore the normal intestinal microflora. Perform an immunity correction. Atherosclerotic vascular changes, which develop in most elderly patients, prevent the flow of drugs to the prostate gland, so special drugs are prescribed to normalize blood circulation.
surgery
There are the following surgical methods for the treatment of prostate adenoma:
- TOUR(transurethral resection). Minimally invasive endoscopic technique. The operation is performed with an adenoma volume below 80 cm3. It is not used in renal failure.
- Adenomectomy.It is performed in the presence of complications, the mass of the adenoma is more than 80 cm3. Currently, laparoscopic adenomectomy is widely used.
- Laser vaporization of the prostate.It allows you to perform an operation with a tumor mass smaller than 30-40 cm3. This is the method of choice for young patients with prostate adenoma, as it allows you to preserve sexual function.
- Laser enucleation(holmium - HoLEP, thulium - ThuLEP). The method is recognized as the "gold standard" of surgical treatment of prostate adenoma. Allows you to remove an adenoma with a volume of more than 80 cm3 without open intervention.
There are a number of absolute contraindications for surgical treatment of prostate adenoma (decompensated diseases of the respiratory and cardiovascular systems, etc. ). If surgical treatment is impossible, bladder catheterization or palliative surgery - cystostomy, placement of a urethral stent - is performed.
Prognosis and prevention
Acute prostatitis is a disease that has a pronounced tendency to chronicity. Even with timely and adequate treatment, more than half of patients end up with chronic prostatitis. Recovery is far from always achieved, but with proper consistent therapy and following the doctor's recommendations, it is possible to eliminate unpleasant symptoms and achieve long-term stable remission in a chronic process.
Prevention is the elimination of risk factors. It is necessary to avoid hypothermia, to alternate sedentary work and periods of physical activity, to eat regularly and wholesomely. Laxatives should be used for constipation. One of the preventive measures is the normalization of sexual life, since both excessive sexual activity and sexual abstinence are risk factors for the development of prostatitis. If symptoms of a urological or sexually transmitted disease appear, you should consult a doctor promptly.























